What is Periodontal Disease?
Periodontal Disease is a highly preventable and treatable, bacterial, chronic inflammatory disease of the gums, that can destroy the bone and connective tissue the supports your teeth.
Plaque that forms below the gum line can irritate the gums and stimulate a prolonged inflammatory response that initiates gingivitis and periodontitis.
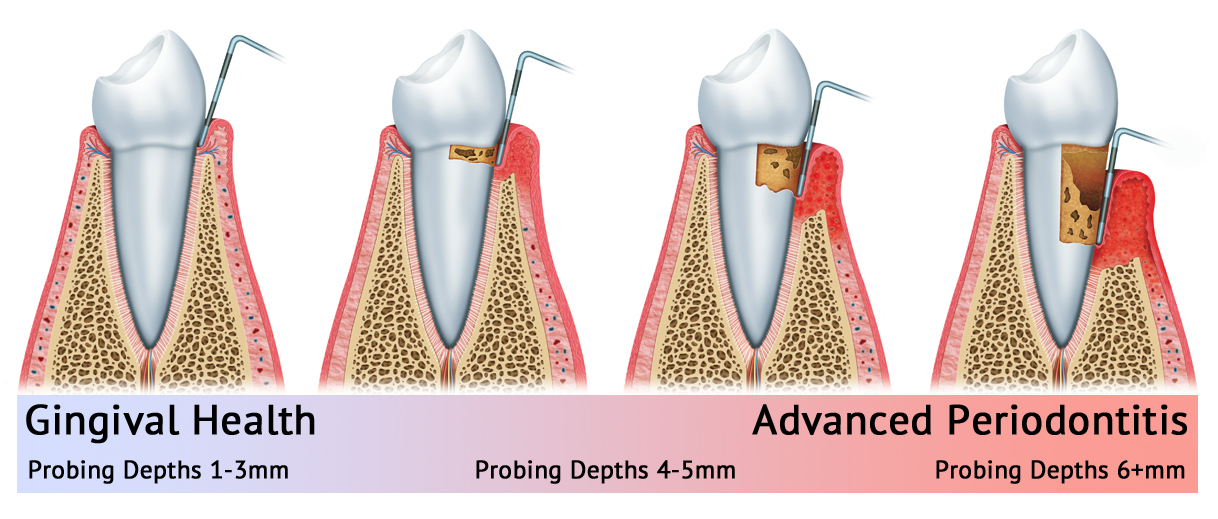
Gingivitis is the mildest form of periodontal disease. Periodontitis is advanced gum disease that occurs if gingivitis is not managed, if oral hygiene is poor, and/or if there is a family history or genetic predisposition. With periodontitis, gums separate from the teeth, forming pockets that become infected with bacteria. Left untreated, this disease can damage the attachment of the teeth to the bone and can eventually destroy gum tissue and bone altogether. The most common type is chronic periodontitis, in which inflammation slowly increases within the supporting tissues of the teeth and progressive detachment and bone loss occurs.
Common Risk Factors
Poor Oral Hygiene
Age
Smoking/Tobacco Use
Genetics
Stress
Medications
Clenching or Grinding Your Teeth
Systemic Disease
Poor Nutrition and Obesity
Symptoms of Periodontal Disease
Red, Swollen or Tender Gums
Bleeding While Brushing, Flossing or Eating Hard Food
Gums That Are Receding or Pulling Away from the Teeth
Loose or Separating Teeth
Pus Between Your Gums and Teeth
Sores in Your Mouth
Persistent Bad Breath
A Change in the Way Your Teeth Fit Together When You Bite
A Change in the Fit of Partial Dentures
Stages and Progression of Periodontal Disease
Periodontal Disease is the Most Common cause of Tooth Loss in Adults.
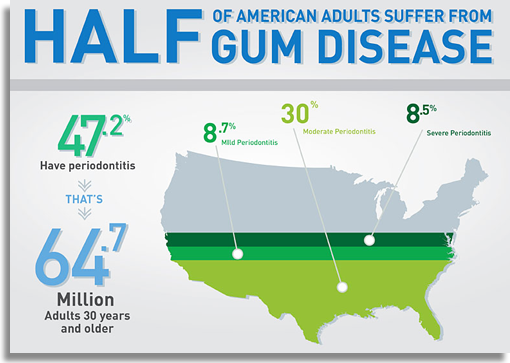
Data from the Centers for Disease Control and Prevention found that “47.2 percent of adults (64.7 million Americans) age 30 and older have periodontal disease”
Learn How You Can Treat Periodontal Disease Before It’s Too Late
Periodontal Disease and Systemic Link
Diabetes
Diabetic patients are more likely to develop periodontal disease, which in turn can increase blood sugar and diabetic complications.
People with diabetes are more likely to have periodontal disease than people without diabetes, probably because people with diabetes are more susceptible to contracting infections. In fact, periodontal disease is often considered a complication of diabetes. Those people who don’t have their diabetes under control are especially at risk.
Research has suggested that the relationship between diabetes and periodontal disease goes both ways – periodontal disease may make it more difficult for people who have diabetes to control their blood sugar.
Severe periodontal disease can increase blood sugar, contributing to increased periods of time when the body functions with a high blood sugar. This puts people with diabetes at increased risk for diabetic complications.

Heart Disease
Several studies have shown that periodontal disease is associated with heart disease. While a cause-and-effect relationship has not yet been proven, research has indicated that periodontal disease increases the risk of heart disease.
Scientists believe that inflammation caused by periodontal disease may be responsible for the association.
Periodontal disease can also exacerbate existing heart conditions. Patients at risk for infective endocarditis may require antibiotics prior to dental procedures. Your periodontist and cardiologist will be able to determine if your heart condition requires use of antibiotics prior to dental procedures.
Stroke
Additional studies have pointed to a relationship between periodontal disease and stroke. In one study that looked at the causal relationship of oral infection as a risk factor for stroke, people diagnosed with acute cerebrovascular ischemia were found more likely to have an oral infection when compared to those in the control group.